What is Plantar Fasciitis?
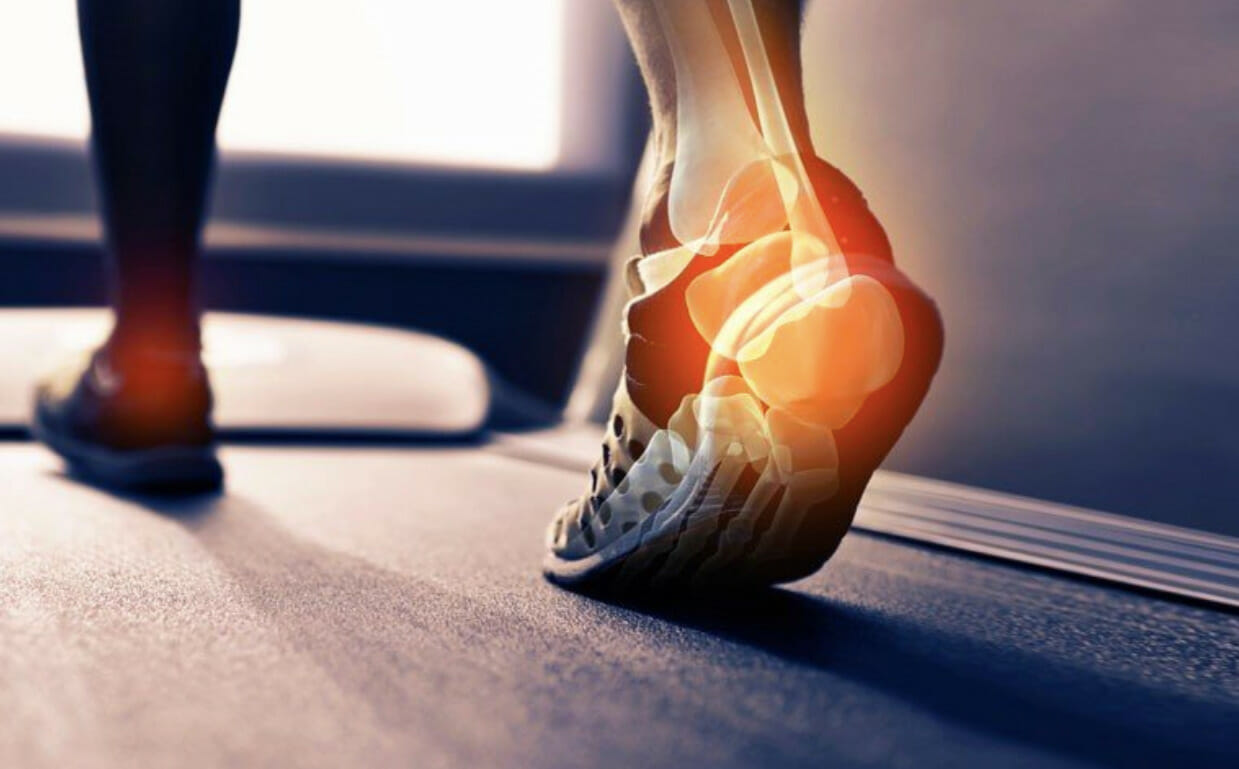
Plantar fasciitis is the leading cause of heel pain, occurring with irritation of a band of tissue located at the base of the foot called the plantar fascia. The plantar fascia plays an important role in the biomechanics of the foot, including dynamic support of the arches, providing shock absorption and creating a stiff lever to propel the body forward with each step. This allows our feet to adapt to different surfaces of terrain and makes walking more efficient.

Symptoms of Plantar Fasciitis
One of the hallmark signs of plantar fasciitis is a sharp pain located on the medial side of the heel, which especially occurs in the first few steps out of bed in the morning. Patients also commonly report the pain goes away once they “walk it out”, where bouts of activity will actually decrease the pain, however this pain starts up again after a period of rest. Plantar fasciitis is the leading cause of heel pain, occurring in around 10% of the general population of predominantly active working adults between 25-65 years of age. The prevalence of this condition is estimated to be as high as 22% in runners.
But common doesn’t mean it’s normal! Plantar fasciitis can often be frustrating to deal with for patients, especially as it can take a while. Since the foot is such an integral part of our daily function, plantar fasciitis can lead to patients taking time off work, sports, and most importantly doing the things they enjoy in their lives.


Causes of Plantar Fasciitis
When the plantar fascia undergoes repetitive strain, overuse or trauma, it can cause micro-tears and degeneration of the tissue resulting in pain at the base of the heel. The causes of this degeneration can be multifactorial. Some predisposing anatomy can include flat or excessively high foot arches and tightness in the calf muscles; these factors can alter how a person regularly loads their feet, hence a greater association with plantar fasciitis.

Risk Factors for Developing Plantar Fasciitis
- Excessively flat or high foot arches
- Running, especially if you increase your running intensity/training quickly
- Leg length discrepancy
- Greater body weight causes greater strain on the feet
- Prolonged standing/walking occupations, especially on hard surfaces and with shoes that have inadequate support
- Sedentary lifestyle
- Tightness of achilles tendon
Heel Spurs and Plantar Fasciitis
Plantar fasciitis is also commonly associated with heel spurs, which are bony growths on the heel that also cause heel pain. Although these can be associated, bone spurs are not the root cause of the plantar fasciitis. The bony growth actually forms as an adaptive response from your calcaneus (heel bone) as a result of the increased tension and painful loading on your heel.

Diagnosing Plantar Fasciitis
Diagnosis of plantar fasciitis can typically be made through a thorough history and physical exam of the foot, and imaging is usually not required to make a clinical diagnosis. There are many causes of foot and ankle pain, and a thorough exam completed by a healthcare professional is important to rule other conditions out, and to provide a recovery program that is unique to your body. If you are suffering from continuous heel or ankle pain, you can book a session with one of our clinicians to have a thorough clinical exam.
Prognosis of Plantar Fasciitis:
Luckily, this condition is not life-threatening or serious. However, it can be very difficult to manage daily activities. We’re on our feet for a lot of our day, and it can be frustrating to deal with persistent pain. Most cases (around 75%) will resolve spontaneously within 12 months. With treatment, this recovery process can be facilitated, and also prevent future recurrences but this process still requires several weeks to months to improve and fully resolve. Since the cause of plantar fasciitis can be multifactorial, treating the root cause of the initial irritation is an important step in recovery and prevention for future occurrences.
Chronic Plantar Fasciitis
Sometimes, more complex cases of plantar fasciitis can be stubborn to treat conservatively. Chronic and complex presentations of this condition may require further or advanced treatments which can include:
- Extracorporeal shockwave therapy
- Steroid injections
- Surgery as the last option if other therapies have failed
Treatment for Plantar Fasciitis
The management of plantar fasciitis will depend on the root causes of the individual’s presentation. A period of relative rest from bouts of running, long periods of standing and walking is generally recommended. Icing after activities can also be helpful for acute pain management.
Conservative treatment, for example a course of physiotherapy including manual therapy, soft tissue work, adequate stretching and exercise prescription should be carried out for 1-2 months. Sometimes plantar fasciitis can resolve on one foot and then develop in the other foot, so prevention for future occurrences is also a huge part of rehab and management.
Appropriate footwear during this time is also an important factor! This will depend on your foot structure (arches, mobility, strength), and what you do throughout the day. However, a supportive and comfortable shoe with a sole that is not too flimsy (which can be comfy, but increases the loading on your foot!) can be helpful for long hours spent standing or walking. A consultation with one of our clinicians may be helpful in determining if you would benefit from custom orthotics that can better support your feet.
Exercises and stretches:
There are also a couple of stretches that can be helpful if you are dealing with heel pain:
- Calf stretches to address achilles tightness

- Rolling frozen water bottle on bottom of foot for pain relief

- Plantar fascia stretch and hold OR toes against wall stretch

Be Patient, and Stay Active!
Last but not least, your body is more resilient than you think! Give yourself rest and patience, but stay active within your own body’s limits. This process looks different for everyone, but remaining active, whether it’s changing up long-distance running for swimming for a while as your foot recovers, or going from sprinting to light jogs. This is a very common condition that takes some work and treatment to resolve – but it CAN be resolved.
5 Myths About Plantar Fasciitis
- Plantar fasciitis means there is a “torn muscle” in my foot
- I have plantar fasciitis because I have a bone spur, so it will never go away unless I have surgery
- Plantar fasciitis only happens because I have flat feet
- There’s no cure for plantar fasciitis
- My plantar fasciitis resolved on its own, so it will never happen again
Book a session with Amy at Bloor West Village or at Spadina today to have a comprehensive clinical exam, or book a free consultation if you have any questions and want to see what our services can offer for you.